Table of Contents
What is Dual Diagnosis?
Dual diagnosis refers to the simultaneous occurrence of a mental health disorder and a substance use disorder. Also known as a co-occurring disorder or co-morbidity, it’s a complex condition that combines two different diagnoses, exacerbating the effects of each. Mental health issues like depression or anxiety intertwine with harmful use of alcohol, drugs, or other addictive substances. This interconnection can create a vicious cycle that intensifies both disorders. If mental health problems are left untreated, substance abuse may worsen; conversely, increased substance use can further destabilize mental health. Breaking this cycle requires specialized treatment, emphasizing an integrated approach to address both disorders concurrently.
Warning Signs of a Co-Occurring Disorder
Recognizing a dual diagnosis can be challenging as signs can vary significantly among individuals, influenced by the substance abused and the severity of the co-existing mental condition. Chattanooga’s leading dual diagnosis treatment center can provide critical insight into identifying such disorders.
Warning signs of dual diagnosis may include:
- Unanticipated shifts in behavior or personality.
- Difficulty in managing routine tasks and obligations.
- Withdrawal from previously enjoyable activities or social events.
- Neglecting of personal health and cleanliness.
- Delusional thoughts or cognitive impairments.
- Resistance to seek or adhere to treatment.
- Expressing suicidal thoughts or demonstrating suicidal behaviors.
- Unpredictable and reckless conduct.
- Poor financial management skills.
- Deteriorating performance at work or academics.
Knowing these symptoms can guide you or a loved one towards the right course of treatment.
How Common is Dual Diagnosis?
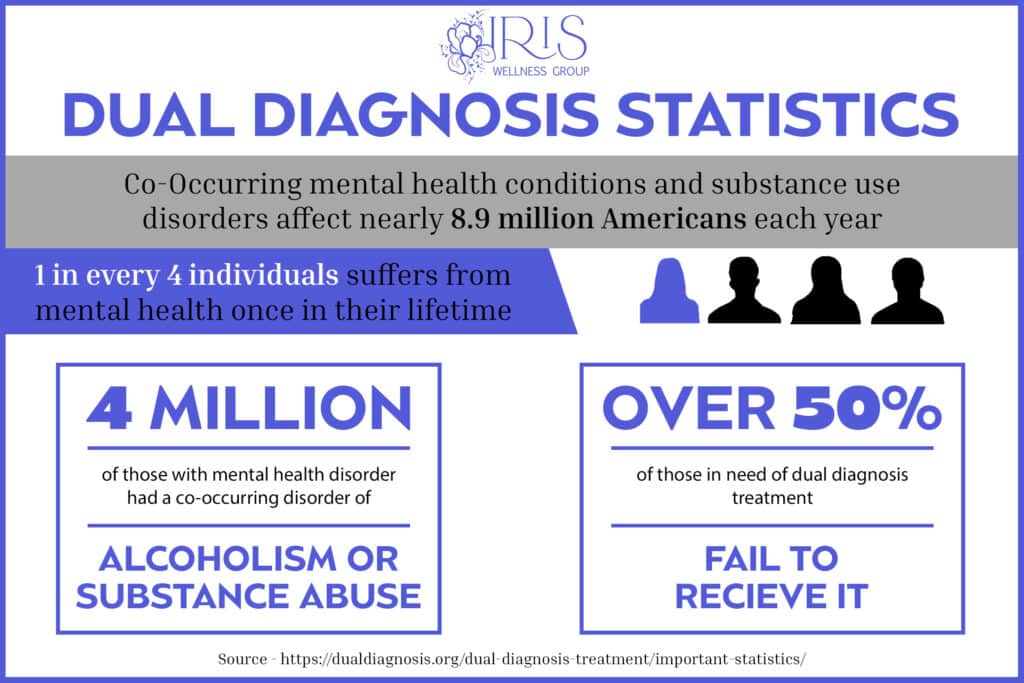
According to SAMHSA’s 2021 National Survey on Drug Use and Health, approximately 9.2 million adults in the United States have a co-occurring disorder. Dual diagnosis, the co-occurrence of mental health disorders and substance abuse, is a relatively common and complex issue. According to some estimates, nearly half of those with a substance abuse disorder also suffer from a mental health condition, and vice versa. This connection can create a vicious cycle where mental health problems lead to substance abuse as a form of self-medication, or where substance abuse exacerbates underlying mental health issues.
The intricacy of dual diagnosis often requires specialized care and an integrated treatment approach to address both aspects simultaneously. Unfortunately, the prevalence of dual diagnosis means that it’s a significant concern in healthcare, making the availability of specialized treatment centers and trained professionals crucial. According to a mental health study, over 50% of those in need of dual diagnosis treatment fail to receive it. The recognition and understanding of dual diagnosis are growing, yet there are still challenges in providing comprehensive care for those affected, due to the complex nature of the intertwined disorders.
Dual Diagnosis Statistics
What are the Symptoms of Dual Diagnosis?
Dual diagnosis refers to the concurrent existence of a substance addiction and a mental health issue, each with unique symptoms. These symptoms vary depending on the specific substances and mental health disorders involved.
Symptoms of a substance use disorder may include:
- Isolation: Withdrawing from family and friends.
- Focus Issues: Difficulty staying concentrated.
- Behavioral Changes: Sudden alterations in behavior.
- Risky Actions: Engaging in dangerous behaviors.
- Tolerance and Withdrawal: Building a high tolerance for the substance and experiencing withdrawal symptoms.
- Dependency: Feeling like you need the substance to function.
Symptoms of a mental health disorder may include:
- Mood Swings: Extreme changes in mood.
- Confusion: Feeling disoriented or perplexed.
- Concentration Problems: Difficulties in focusing or thinking clearly.
- Functional Issues: Struggles with work or school responsibilities.
- Social Withdrawal: Avoidance of social activities or interactions.
- Suicidal Thoughts: Having thoughts or making plans about suicide.
Understanding these symptoms can be vital in identifying and treating a dual diagnosis effectively.
Common Mental Health Issues and Addiction
At the top dual diagnosis treatment center in Chattanooga, Tennessee, individuals struggling with addiction are offered the chance to comprehend and delve into frequent mental health problems linked to substance abuse. This relationship between mental health and addiction is a complex one, where certain mental health disorders can actually lead to addiction, or even exacerbate it.
Ignoring the symptoms of mental health conditions or behavioral disorders while planning addiction recovery can lead to challenges in the long run. The integration of care for both mental health issues and addiction is vital for a comprehensive recovery strategy.
These are some prevalent mental health disorders that have a connection to substance abuse:
- Attention-Deficit Hyperactivity Disorder (ADHD): Those with ADHD may resort to drugs to alleviate symptoms, particularly when prescribed stimulants, which might become addictive.
- Bipolar Disorder: Nearly half of those with bipolar disorder face addiction issues, often seeking solace from emotional turmoil or manic phases through drugs or alcohol.
- Borderline Personality Disorder (BPD): Addiction frequently co-occurs with BPD, with over two-thirds of BPD sufferers having abused substances at some stage.
- Depression: Attempting to self-treat depression with drugs or alcohol can exacerbate the condition over time.
- Eating Disorders: Substance abuse is common among people with eating disorders as they may use appetite-suppressing drugs.
- Generalized Anxiety Disorder (GAD): GAD sufferers might turn to drugs, alcohol, or misuse prescription medications like Benzodiazepines to handle symptoms.
- Obsessive-Compulsive Disorder (OCD): Those with OCD may resort to drugs or alcohol to mitigate anxiety and depression related to their unwanted obsessions and compulsions.
- Post-Traumatic Stress Disorder (PTSD): PTSD often leads people to drugs or alcohol as the brain produces fewer feel-good chemicals after trauma.
- Schizophrenia: Diagnosing addiction with schizophrenia is difficult due to their similar effects. Substance abuse can put the health of a schizophrenic patient at a greater risk.
To develop an effective, long-lasting recovery plan, it is of upmost importance to treat both the addiction and any underlying mental health issues simultaneously. Understanding the symbiotic relationship between mental health disorders and addiction aids in customizing treatment plans at our dual diagnosis treatment center in Tennessee, ensuring a well-rounded and thorough approach to healing and recovery.
The partnership between mental health issues and substance abuse is intricate, but recognizing the underlying causes and the connections between them forms the bedrock of a sound, holistic recovery strategy. It’s not merely about treating addiction but addressing the person as a whole, exploring the underlying mental health issues that might have led to or been exacerbated by substance abuse. This comprehensive approach ensures lasting healing, equipping clients with the tools and understanding they need for lifelong stability and health.
Treatment Options for Dual Diagnosis in Chattanooga, TN
At Chattanooga, TN’s premier mental health treatment center, clients have access to a broad spectrum of therapeutic options tailored to their needs. A successful remedy for co-occurring disorders, such as addiction combined with mental health issues, requires a simultaneous, integrated approach. This means both the addiction and mental health disorder must be addressed concurrently, weaving them into a cohesive treatment plan. Long-term recovery depends not on which issue appeared first, but on addressing both the mental health and substance abuse challenges together. Treatment must be coordinated by a unified provider or team to ensure consistent and thorough care.For mental health treatment, the individualized treatment may encompass:
- Prescription Medications
- Individual Counseling
- Group Therapy Sessions
- Self-Help Strategies
- Lifestyle Modifications
- Peer Support
For substance abuse treatment, the personalized treatment approach may include:
- Detoxification Process
- Management of Withdrawal Symptoms
- Behavioral Therapy Interventions
- Engagement in Support Groups to Sustain Sobriety
Why Is Self-Medication Dangerous?
Facing both mental illness and substance use requires specialized care, like that offered at Chattanooga, TN’s best dual diagnosis treatment program. People often use drugs and alcohol to deal with mental illness, seeking temporary relief. However, this can lead to addiction or even overdose as the effects wear off and the need to use them grows. Addressing both mental health symptoms and addiction makes treatment more complicated. A dual diagnosis treatment center is key to tackling both problems effectively, cutting the risk of future relapse. It’s not just about treating the addiction but understanding the underlying mental issues that may have led to or worsened it. This approach ensures a path towards a healthier life.Our Dual Diagnosis Treatment Center in Chattanooga, TN
Iris Wellness Group is one of the best dual diagnosis treatment centers in Tennessee, specializing in the treatment of both mental health & substance use disorders. If you or someone you care about might be suffering from alcoholism, don’t wait for recovery to start. Iris Wellness Group’s alcohol and drug rehab in Chattanooga, Tennessee treatment center can help today. We’ll meet with you and your family members to honestly assess the situation and develop a personalized path to sobriety. We specialize in Alcohol Use Disorder and can work with you immediately.Dual Diagnosis Frequently Asked Questions
What Is Dual Diagnosis Treatment?
Dual diagnosis treatment addresses both a mental health disorder and a substance abuse issue simultaneously. It involves a comprehensive approach that includes therapy, medication management, and support services. This integrated treatment is crucial because treating one condition while neglecting the other can hinder overall recovery.
What Does Dual Diagnosis Mean?
Dual diagnosis refers to the co-occurrence of a mental health disorder and a substance use disorder. Individuals with dual diagnosis require a specialized treatment approach that addresses both conditions as interconnected issues.
What Is a Dual Diagnosis Treatment Center?
A dual diagnosis treatment center offers specialized care for individuals with co-occurring mental health and substance use disorders. These centers provide integrated treatment plans, including therapy, medical management, and support services, tailored to address the complexities of dual diagnosis.
What Is the Best Treatment for Dual Diagnosis?
The best treatment for dual diagnosis is an integrated approach that simultaneously addresses mental health and substance abuse issues. This typically involves a combination of medication, individual and group therapy, and support groups, tailored to the individual’s specific needs.
What Is Dual Diagnosis Group Therapy?
Dual diagnosis group therapy involves structured group sessions where individuals with co-occurring disorders can share experiences, offer mutual support, and learn coping strategies. It’s facilitated by a therapist and focuses on topics relevant to dual diagnosis recovery.
What is a Dual Diagnosis Intensive Outpatient Program
A dual diagnosis intensive outpatient program (IOP) offers structured therapy and support for individuals with dual diagnosis, allowing them to live at home while receiving treatment. It includes regular sessions focused on both mental health and substance abuse recovery.
How Much Does a Dual Diagnosis Outpatient Treatment Program Cost?
The cost of a dual diagnosis outpatient treatment program varies based on factors like program length, frequency of sessions, and the types of services provided. Insurance may cover some costs, but it’s important to check with your provider for specific coverage details.
How Can I Find Dual Diagnosis Outpatient Treatment Near Me?
To locate dual diagnosis outpatient treatment near you, start by searching online for “dual diagnosis treatment near me” or “dual diagnosis rehab near me.” This will provide a list of nearby facilities offering specialized care for co-occurring disorders. Additionally, you can ask for referrals from your healthcare provider or local mental health clinics. It’s important to choose a program that fits your specific needs, offers comprehensive care, and is conveniently located to ensure consistent attendance and effective treatment.
Who is Chattanooga Anxiety Treatment Designed For?
Chattanooga dual diagnosis treatment caters to individuals living in Chattanooga, Red Bank, Signal Mountain, Lookout Mountain, Southeastern Tennessee, Northern Georgia, or surrounding areas. These services are ideal for those who do not require medically supervised detoxification, have a stable and supportive home and work environment, and are self-motivated in their journey towards recovery.
What's the Difference Between Dual Diagnosis and Co-Occurring Disorder?
The terms ‘dual diagnosis’ and ‘co-occurring disorder’ are often used interchangeably. Both refer to a situation where an individual simultaneously experiences a mental health disorder and a substance use disorder. However, ‘dual diagnosis’ can sometimes be used more broadly to refer to the presence of any two co-occurring conditions, not limited to substance use.
What Is Dual Diagnosis for Mental Health?
In mental health, dual diagnosis refers to the coexistence of a mental health disorder, such as depression, anxiety, or bipolar disorder, along with a substance use disorder. This condition requires an integrated treatment approach that addresses both the mental health issue and the addiction to ensure effective recovery.
What Is the Dual Diagnosis Model of Treatment?
The dual diagnosis model of treatment is an integrated approach that simultaneously addresses a person’s substance abuse and mental health disorders. This model recognizes that both disorders are interlinked and that effective treatment must involve comprehensive care, including therapy, medication management, and support services, tailored to treat both conditions in a coordinated manner.